Breakthrough in Indian Orthopaedic Care Asian Orthopaedic Institute Unveils Advanced Hip Surgery Facility and Innovative Technologies For the First Time…
Orthopaedics
WE BUILD CONNECTIONS WITH ORGANIZATIONS AND COOPERATE WITH SMART PEOPLE ALL OVER THE WORLD
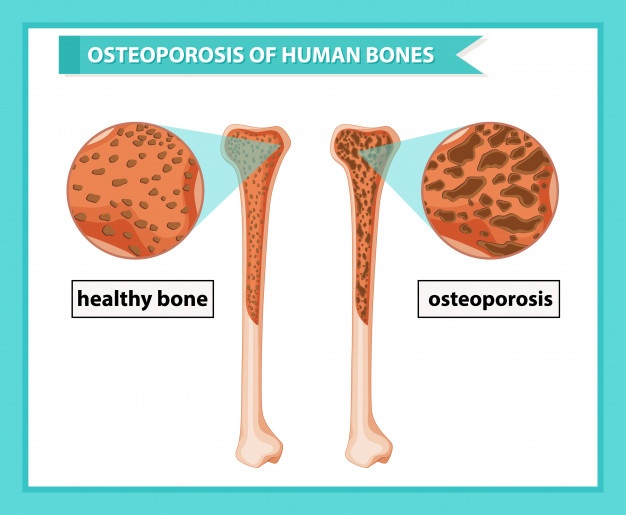
Osteoporosis What is Osteoporosis? Osteoporosis means “porous bone.” Bones are porous or weaker in people with osteoporosis, which increases the…
Musculoskeletal Disorders Also known as MSDs, Musculoskeletal disorders, account for several conditions that require days away from work. It is…
You Can Walk Again ! ALL ABOUT OSTEOARTHRITIS AND TOTAL KNEE REPLACEMENT According to the National Health Portal Osteoarthritis is…