- No products in the cart.
Institute Of
Gastroenterology
Home » The Institute of Gastroenterology, Hepatobiliary Science & Transplantation » Surgical Gastroenterology » GI Bleeding Surgery
GI Bleeding Surgery
GI Bleeding is a critical condition where patients mostly encage with massive vomiting of blood or hematemsis. Some of the most general causes of GI bleed are cirrhosis of liver and ulcer disease. Bleeding stops on its own in 90% of the patients. The remaining will either need endoscopic treatment or sometimes surgery to effectively stop the bleeding. GI bleeding can be life threatening if not treated on time. It is predominantly characterized by hemorrhage in the GI tract starting from the pharynx down to the rectum.
GI bleed may be extensively categorised as higher GI and decrease GI bleed. Upper GI bleed originates from the pharynx and ligament of Treitz. Lower GI bleed originates from the colon, rectum or anus
Where the reasons are showed as peptic ulcer, gastric erosions because of alcohol and NSAIDs, gastric varices, Mallory-Weiss tear, angiodysplasia and gastric cancers the subsequent surgical are recommended:
Under-running the ulcer:
Peptic ulcers generally prevent bleeding spontaneously. But while non-operative strategies fail, surgical operation turns into the simplest alternative for a life-threatening situation. The most effective manner to prevent an ulcer from bleeding is to by under running it. The surgery is done under general anesthesia. The laparoscopic procedure involves making a 11mm port just under the xiphisternum. 2 to 3 stitches are exceeded deep into the ulcer and the sutures are tied tight to prevent the bleeding. A major part of the process involves just looking for the peptic ulcer which is an exceptionally tedious and meticulous process.
Pyloroplasty :
A pyloroplasty is done to open the lower part of the stomach, a thick area of muscle known as pylorus. Under general anesthesia, a laparoscopic operation requires three small incisions between the stomach and duodenum. Part of the thickened muscle of the pylorus is divided and cut laterally to widen it, making the connection larger. There are at least three types of pyloroplasty:
- Jaboulay pyloroplasty Without pylorus incision – side to side gastroduodenostomy
- Heineke Mikulicz pyloroplasty longitudinal incision transversely across the pylorus – common procedure
- Finney pyloroplasty With pylorus incision – side to side gastroduodenostomy
Partial gastrectomy
During this procedure, part of the stomach is removed. The procedures are performed under general anesthesia. A midline incision from the xiphoid process to the umbilicus and self-maintaining subcostal retractors the upper abdomen is explored for metastasis.The portion of the stomach is resected and a gastroduodenal anastomosis is performed after duodenal and omental mobilization
Total gastrectomy :
This procedure aims at cutting into the abdomen to resect all of the stomach. A midline or bilateral subcostal incision is made below the umbilicus to expose the stomach and distal esophagus. Self-retaining retractors provide a wider exposure. The stomach is retracted and the esophagus is directly connected to the small intestine.
Vagotomy :
The vagus nerve which is also known as pneumogastric nerve is resected. There are of many types including:
- Truncal vagotomy, first the pylorus is drained and then separated from the main trunk of the vagus.
- Selective vagotomy, in this process the pylorus is first drained and then the anterior and posterior nerves of Latarjet are separated.
- Highly selective vagotomy, also known as proximal gastric vagotomy and involves denervation of the fundus and stomach
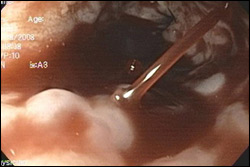
Endoscopic variceal ligation (EVL) :
For patients who present with bleeding from esophageal varices (swollen veins in the food pipe), endoscopic variceal ligation is the treatment of choice and surgery is usually performed as a last resort if all other measures fail.
The procedure is performed endoscopically when an enlarged vein or varix in the esophagus is tied off with a rubber band. In view of the poor liver condition these patients are not good candidates for surgery.
Non-cirrhotic patients are those with portal vein thrombosis or non-cirrhotic portal vein fibrosis, which are also an important component of gastrointestinal bleeding. These patients are doing very well after the operation due to their preserved liver condition.
The procedure is performed endoscopically when an enlarged vein or varix in the esophagus is tied off with a rubber band. In view of the poor liver condition these patients are not good candidates for surgery.
Non-cirrhotic patients are those with portal vein thrombosis or non-cirrhotic portal vein fibrosis, which are also an important component of gastrointestinal bleeding. These patients are doing very well after the operation due to their preserved liver condition.
Splenorenal shunt and splenectomy with devascularisation :
Some patients presenting with intermittent vomiting of blood or passing melena will require surgical treatment as a permanent cure for bleeding. The operation takes the form of a splenorenal bypass in non-cirrhotic patients or a splenectomy with devascularization in cirrhotic patients.
- Splenorenal shunt : In a splenorenal shunt procedure,the spleen vein is separated from the portal vein and opens into the renal vein, which reduces varicose veins.
- Splenectomy and devascularization : New procedures for splenectomy and devascularization require that a splenectomy is performed first. The distal esophagus is then devascularized through the diaphragm hiatus.
The Institute of Gastroenterology is one among the most effective bariatric surgeons in Chennai. Our specialists has tremendous experience in Gastro-intestinal bleeding surgery. Dr. Radhakrishna has presented his expertise in portal hypertension surgery in many national and international conferences, including the 2010 Asia Pacific Hepatobiliary Conference in Bangkok and Digestive Disease Week in New Orleans, USA.

